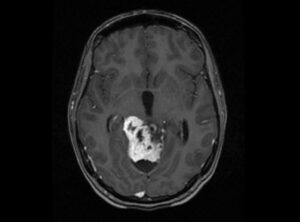
 Radiation therapy (RT) is one of the most common and effective cancer treatments, used in over half of cancer patients. But for some tough cancers, like glioblastoma multiforme (GBM), RT has its limitations. This is because these tumors often have areas with low oxygen (hypoxia), suppress the immune system, resist radiation, and are close to healthy tissue that can’t tolerate high doses.
Radiation therapy (RT) is one of the most common and effective cancer treatments, used in over half of cancer patients. But for some tough cancers, like glioblastoma multiforme (GBM), RT has its limitations. This is because these tumors often have areas with low oxygen (hypoxia), suppress the immune system, resist radiation, and are close to healthy tissue that can’t tolerate high doses.
Traditional radiation tries to give the entire tumor the same amount of radiation, but new research shows that delivering radiation in patterns with high- and low-dose regions—called spatially fractionated radiation therapy (SFRT)—can actually kill tumor cells more effectively and activate the immune system while sparing healthy tissue. One version of this, called minibeam radiation therapy (MBRT), has shown great promise in animals and early human studies.
Several research groups are now exploring combining MBRT with proton therapy (which uses proton particles rather than X-rays) because protons can target tumors more precisely and penetrate deeper without affecting tissue beyond the tumor. However, this combination (pMBRT) is still in early stages of development. One big challenge in treating tumors is their low oxygen levels, because oxygen helps radiation create molecules that damage cancer cells’ DNA. Tumors with little oxygen are much harder to treat. In addition, oxygen levels can affect the immune response and even harm normal brain function when used during anesthesia in radiation treatments.
Researchers in France set out to find out whether pMBRT could overcome the problem of low oxygen, while also maintaining effectiveness against the tumor, supporting immune responses, and avoiding cognitive side effects and healthy tissue damage. They tested this in rats with brain tumors and in healthy animals, to better understand how oxygen levels in the blood influence outcomes. The differential effects of blood oxygenation were assessed by analyzing immune response, survival capability, and histopathological changes in brain and bone tissues.
Using micro computed tomography (microCT) the researchers used the Analyze Bone Microarchitecture Analysis (BMA) software as well as semi-automatic and manual segmentation tools to assess bone structure, measuring parameters like bone volume, bone thickness and Hounsfield unit distribution.
The study revealed that following pMBRT, no significant influence of oxygen supplementation on survival outcomes or immune infiltration were present. Also, no significant brain or bone tissue alterations were observed, regardless of blood oxygenation levels during irradiation. These findings highlights the promise for pMBRT in glioblastoma treatment compared to CPT and conventional radiation therapy.
Additional resources:
>> Analyze 15.0 User’s Guide: Bone Microarchitecture Analysis (BMA)
>> Analyze 15.0 Help Videos: Bone Microarchitecture Analysis (BMA).
 AnalyzeDirect
AnalyzeDirect